Introduction
Tubectomy, commonly known as female sterilization, is a permanent method of birth control widely used by women around the world. This surgical procedure involves blocking or cutting the fallopian tubes to prevent eggs from reaching the uterus, thereby preventing pregnancy. Despite its effectiveness, there are numerous aspects of tubectomy that individuals need to consider before opting for this form of contraception. In this blog, we will delve deep into what tubectomy entails, how it compares to vasectomy (the male counterpart), the procedure involved, recovery time, and other essential details that can help in making an informed decision.
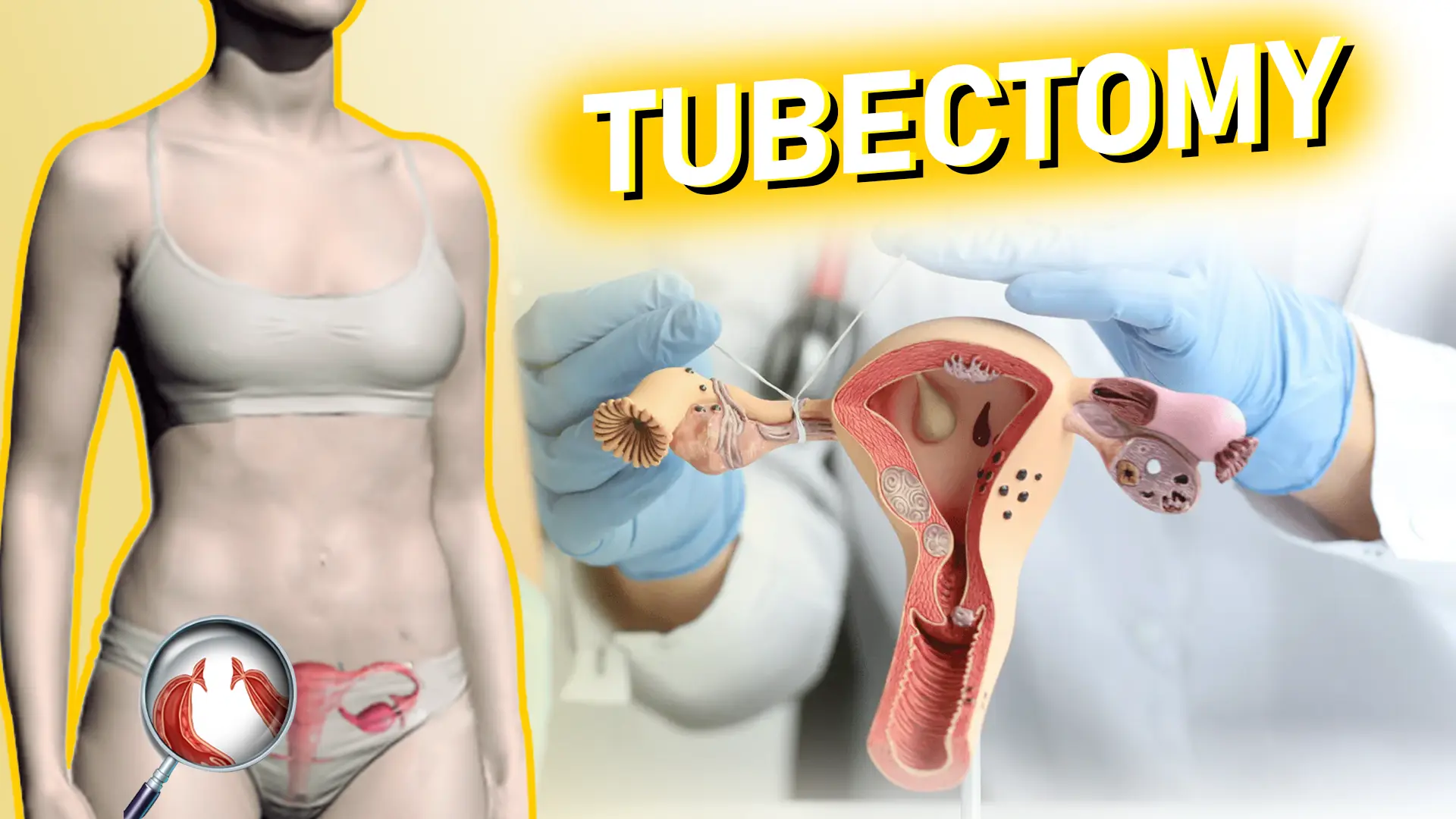
What is Tubectomy?

Tubectomy is a surgical procedure that involves the severance or blockage of the fallopian tubes, which connect the ovaries to the uterus. This process prevents the eggs released by the ovaries from traveling through the fallopian tubes and being fertilized by sperm. Consequently, this prevents pregnancy.
The Anatomy Involved
To understand tubectomy, it’s crucial to have a basic understanding of female reproductive anatomy:
- Ovaries: Two small glands that produce eggs (ova) and hormones like estrogen and progesterone.
- Fallopian Tubes: These are the tubes that transport the eggs from the ovaries to the uterus.
- Uterus: The organ where a fertilized egg implants and grows into a fetus.
During a tubectomy, the fallopian tubes are either cut, tied, or blocked permanently to ensure that sperm cannot meet the egg.
Why Opt for a Tubectomy?
There are various reasons why a woman might choose tubectomy as a form of contraception:
- Permanent Solution: Tubectomy is ideal for women who are certain they do not want more children or any children at all.
- Highly Effective: It is one of the most effective forms of birth control, with a success rate of over 99%.
- Convenience: Unlike temporary contraceptive methods, tubectomy does not require regular attention or ongoing costs.
Comparing Tubectomy and Vasectomy
A common question that arises is how tubectomy compares to vasectomy, the male sterilization procedure. Understanding both can help couples make a more informed decision.
What is Vasectomy?
A vasectomy is a surgical procedure for male sterilization that involves cutting or sealing the vas deferens, the tubes that carry sperm from the testicles to the urethra. By preventing sperm from mixing with semen, a vasectomy ensures that ejaculation does not lead to pregnancy.
Tubectomy vs. Vasectomy
- Complexity of Surgery: A vasectomy is generally simpler, less invasive, and has fewer complications compared to tubectomy. It is usually performed under local anesthesia, whereas tubectomy often requires general anesthesia.
- Recovery Time: Recovery from a vasectomy is typically quicker, with most men returning to normal activities within a few days. Tubectomy, being a more complex procedure, usually requires a longer recovery period.
- Risks and Complications: Both procedures are safe, but tubectomy carries a slightly higher risk of complications due to the nature of the surgery.
- Effectiveness: Both tubectomy and vasectomy are equally effective in preventing pregnancy.
Tubectomy Operation: What to Expect
Pre-Operation Preparation
Before undergoing a tubectomy, there are several steps involved in preparation:
- Consultation: A thorough consultation with a healthcare provider is crucial. This will involve discussions about medical history, the reasons for choosing tubectomy, and potential alternatives.
- Medical Tests: Some routine tests might be required to ensure the patient is fit for surgery, including blood tests, pregnancy tests, and possibly an ultrasound.
- Consent: Since tubectomy is a permanent procedure, patients are often required to sign a consent form acknowledging that they understand the implications.
The Procedure
A tubectomy can be performed using various techniques, but the most common methods are laparoscopic tubectomy and mini-laparotomy.
- Laparoscopic Tubectomy: This is a minimally invasive procedure where a laparoscope (a thin tube with a camera) is inserted through a small incision in the abdomen. The surgeon then blocks or cuts the fallopian tubes using specialized instruments.
- Mini-Laparotomy: This is a slightly more invasive procedure involving a small incision in the abdomen through which the fallopian tubes are accessed and blocked or cut.
- Post-Partum Tubectomy: Sometimes, tubectomy is performed immediately after childbirth, especially after a C-section. This method is convenient as the patient is already in the hospital, and no additional anesthesia is required.
Recovery After Tubectomy
Post-operative care is crucial for a smooth recovery. Here are the key aspects of the recovery process:
- Immediate Post-Op Care: Patients are usually kept under observation for a few hours post-surgery to monitor for any immediate complications. Pain and discomfort are common, and pain relievers are prescribed.
- Bed Rest: One of the most common questions is, “How many days bed rest after a tubectomy?” Generally, bed rest is recommended for at least 2 to 3 days following the surgery. However, the total recovery time can vary depending on the individual and the type of procedure performed.
- Resuming Normal Activities: Most women can return to light activities after about a week, but it’s advised to avoid heavy lifting, strenuous exercise, or sexual intercourse for a few weeks. Full recovery might take up to 4-6 weeks.
- Follow-Up: A follow-up visit is usually scheduled a week or two after the surgery to ensure proper healing and address any concerns.
Potential Risks and Complications
While tubectomy is generally safe, as with any surgical procedure, there are potential risks and complications that one should be aware of:
- Infection: Post-operative infection can occur at the incision site or internally, though it is rare. Antibiotics are usually prescribed to prevent this.
- Internal Bleeding: There is a small risk of internal bleeding, particularly if the surgery was complicated.
- Failure: In rare cases, the fallopian tubes may naturally heal and rejoin, leading to a possible pregnancy, including the risk of ectopic pregnancy.
- Anesthesia Risks: As with any procedure requiring anesthesia, there is a risk of adverse reactions, though this is very rare.
- Emotional Impact: Some women may experience emotional or psychological effects after the procedure, particularly if they were uncertain about their decision. Counseling is recommended for women who are unsure.
Reversing Tubectomy: Is It Possible?
One of the key considerations before opting for a tubectomy is understanding that it is intended to be a permanent form of contraception. However, some women may later regret their decision and wish to have the procedure reversed.
Tubal Reversal Surgery
Tubal reversal, or tubal reanastomosis, is a procedure that attempts to restore fertility by reconnecting the severed or blocked fallopian tubes. The success of this surgery depends on several factors:
- Type of Tubectomy: The method used in the original tubectomy can affect the chances of successful reversal.
- Age: Younger women generally have a higher chance of a successful reversal.
- Time Since Tubectomy: The longer the time since the tubectomy, the lower the chances of a successful reversal.
- Overall Health: The woman’s overall health and reproductive health play a crucial role in the success of the reversal.
Even with successful surgery, the chances of pregnancy may not return to the levels they were before the tubectomy. Additionally, there is an increased risk of ectopic pregnancy after tubal reversal.
Alternatives to Tubectomy
For women who are uncertain about permanent sterilization, there are several alternative contraceptive methods to consider:
- Intrauterine Devices (IUDs): These are long-term, reversible forms of contraception that can be removed if a woman decides to become pregnant.
- Hormonal Contraceptives: Birth control pills, patches, injections, and implants are effective but require ongoing use.
- Barrier Methods: Condoms, diaphragms, and cervical caps are non-permanent options that prevent sperm from reaching the egg.
- Natural Family Planning: This involves tracking the menstrual cycle to avoid sex on fertile days but is less reliable.
- Vasectomy: As discussed earlier, vasectomy is a simpler, less invasive alternative for couples considering permanent birth control.
Social and Ethical Considerations
Tubectomy, like other forms of permanent contraception, carries significant social and ethical implications. In many cultures, the decision to undergo sterilization is influenced by factors such as:
- Cultural Norms: In some societies, women may feel pressured to undergo sterilization after having a certain number of children, often due to societal or familial expectations.
- Access to Information: The availability of comprehensive information about the procedure and its consequences is crucial. Women should be fully informed about all their options before making a decision.
- Informed Consent: Ensuring that women are not coerced into sterilization and that they fully understand the permanency of the procedure is a critical ethical concern.
- Economic Factors: In some cases, economic incentives or pressures may play a role in the decision to undergo tubectomy, particularly in regions where large families may be seen as a financial burden.

